Can supplements really help with mental health?
Short answer : Yes.
Longer answer : Clinical doses of specific nutraceuticals, namely broad-spectrum vitamin and mineral formulations, have shown a significant reduction of symptoms in depression and anxiety in many population groups in many circumstances.
Interestingly, there appears to be significant variation between individual responses. Many of the studies noted a sub-population of ‘super-responders’, i.e. some who respond really well, yet others who show a modest or no response, unrelated to baseline blood micronutrient levels. This is believed to be due to genetic variation within subjects, predisposing some to require high dose micronutrients to optimise brain and body metabolic pathways, which is then corrected by supplementation, alleviating symptoms.
If they work, then why are they not prescribed by GPs?
There is not yet the level of evidence required for nutraceuticals to be included in clinical guidelines in the UK. There are many reasons for this which will be discussed in another blog: ‘The challenges of Nutrition research’, but mostly due to study design and the fact that different formulations, doses & regimens have been used in randomised controlled trials (RCTs) so researchers can’t pool that data to conduct the meta-analyses required to be eligible for guideline inclusion.
How do they work?
Vitamins and minerals are crucial in the pathways for the synthesis and metabolism of the neuromodulators serotonin and dopamine, imbalances and deficits of which are believed to be contributory factors in depression, anxiety and other mood disorders.
Those of us who are genetically predisposed to mental health conditions are believed to have gene polymorphisms which result in a mild or dramatic reduction of the functioning of certain enzymes, impairing the metabolic pathways that play a crucial role in mental health. These gene polymorphisms can be inherited and/or caused by our environment (epigenetics). Clinical doses of the enzyme cofactor vitamins and minerals have been shown to correct enzyme impairments.
How does that work?
Enzymes are needed to break down or build up substances in the body. They are involved in all metabolic pathways. Most enzymes cannot function without their cofactor(s). Clinical doses of cofactor minerals and vitamins appear to restore the function of ‘sluggish’ enzymes to normal levels, thereby optimising serotonin, dopamine and other metabolic pathways, and alleviating depression and anxiety.

.

In addition to serotonin and dopamine, other neurotransmitters and neuromodulators require vitamins and minerals as enzyme cofactors to optimise their metabolic pathways, including that of GABA (pathway impairment is believed to be a causal factor in anxiety and mood disorders) which requires B6 as a cofactor.
The Liver
It’s not just in the brain. Other metabolic pathways are known to impact mental health too. Such as the detoxification pathway in the liver; many vitamins & minerals are essential cofactors for liver enzymes to break down toxins from our diet, environment and those made in our bodies. If these enzymes are inhibited by herbicides or are ‘sluggish’ due to gene polymorphisms then this leaves a high toxic load in our blood which may cross the blood brain barrier and cause neuroinflammation in our brain contributing to depression, anxiety and mood disorders.

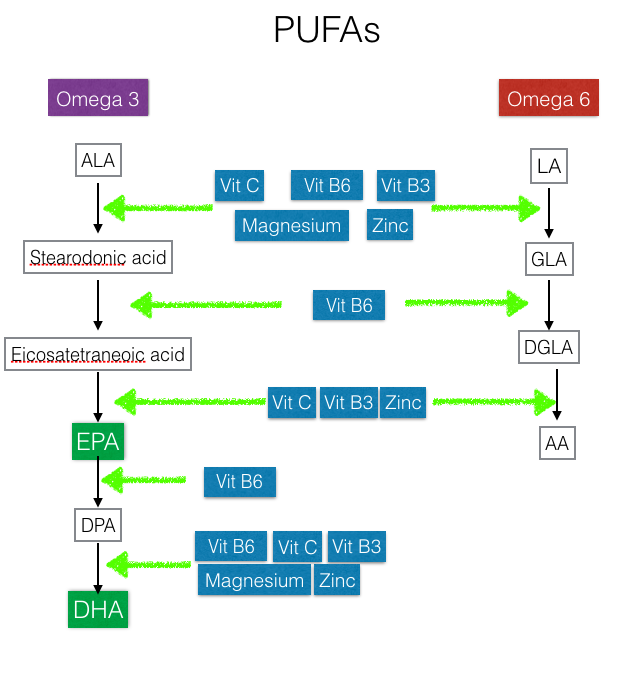
Omega 3 & Omega 6
Poly Unsaturated Fatty Acids PUFAs Omega 3 and 6 have many important roles for optimising brain function and mental health, particularly the metabolites of Omega 3s – EPA & DHA. Cell membranes function better when they are comprised of EPA and DHA rather than trans fats, and it seems that they preserve the integrity of the blood brain barrier (although only studied in mice so far). Their metabolic pathways are determined by the availability of many minerals and vitamins, which may explain why the beneficial effects seen from Omega 3 supplementation are greater when given alongside clinical doses of broad spectrum minerals and vitamins.
Mitochondria
The mitochondria are the batteries of our bodies. They are present in every cell and give the cell the energy to function. They rely on virtually every vitamin and mineral as cofactors for enzymes in their metabolic pathways. The nerve cells in our brains use significantly more energy than other body cells so it’s crucial that our brain cells have a plentiful supply of all the vitamins and minerals involved.

The blue boxes show the sheer number of vitamins and minerals required for mitochondria to function optimally.
Methylation
A process called methylation is also heavily dependent on adequate consumption of vitamin and mineral cofactors, with an increased requirement if there is a genetic impairment in enzyme function in this cycle. The effectiveness of the methylation cycle determines which genes get switched on and which don’t. Impaired methylation in those genetically predisposed to certain diseases, can result in those disease genes being switched on, rather than off, and also for enzymes to be switched on or off.
Methylation happens to DNA, hormones, immune cells and neurotransmitters (repairing DNA damage, damaged cell membranes etc) and occurs billions of times every second! Impairment in the methylation cycle not only directly affects the function of neuromodulators such as serotonin and dopamine but also leads to inflammation in the body and brain further impacting mental health.
Don’t I need to be deficient in the vitamins and minerals to see an effect?
No. The fallacy that we need to be deficient in certain vitamins or minerals to see a benefit from supplements is false.
Why?
Firstly, if we’re taking blood tests to measure levels, this is extremely limited. Plasma levels of vitamins and minerals only really reflect the mineral and vitamin content of what we have absorbed from a recent meal. Red blood cell measures are a closer estimate but still only determine what is present in the blood which often bears little relation to what is in other body compartments, such as the brain, the muscle, adipose tissue and most importantly what is actually inside cells.
And secondly, if we’re trying to estimate deficiencies from dietary intake and corresponding Recommended Daily Allowances RDAs or Dietary Reference Intake DRIs this is also deeply flawed for a number of reasons. RDAs + DRIs were arbitrarily calculated to avoid symptomatic deficiency (eg scurvy due to lack of Vitamin C, or rickets due to lack of Vitamin D), they were not developed as guides to optimise metabolic and/or brain health. Plus, the vitamin and mineral content of foods is often significantly lower than estimates (based on historical data) due to mineral depleted soils, herbicides blocking crop absorption of minerals and therefore lower vitamin and mineral content of foods. Also, what we eat is not what we absorb, and common conditions associated with the western diet such as gut dysbiosis and gut inflammation significantly reduce vitamin and mineral absorption.
Thirdly and most interestingly, in the studies of clinical vitamin and mineral supplementation for mental health conditions, where baseline blood levels were recorded, there was equal benefit in those who were deficient and in those (most) whose blood levels were in the desired range. In fact, some outcomes were far superior if there was no deficiency in certain vitamins (eg Vitamin D) and minerals (iron) to start with.
Can’t I just take an off the shelf ‘one a day’ multivitamin and mineral supplement?
No, these products have much lower doses of minerals and vitamins than the clinical levels used in the studies, and generally have significantly lower bioavailability (ability to be absorbed in the body) than the formulations used in the studies. Also, most supplement manufacturers do not have standardised quality control measures in place so the active ingredients are often at lower doses than stated or not present at all.
Summary
Overall, in many population groups: children, teens and adults, for symptoms of anxiety and depression, studies have shown on average, a significant improvement in symptoms across the population group studied, often with a few responding dramatically to the point of remission (42% in one study in depression), most reporting some benefit, and few not responding at all. They were well tolerated with minimal or no side effects. Effects were greater the broader the spectrum of vitamins and minerals. The studies where no difference was observed between treatment and placebo, did not include the full spectrum of vitamins and minerals.
More research is needed to identify the sub-groups who are most likely to respond well, and more research is needed to determine the optimal duration of treatment. It is likely that in many studies, outcomes would have been even greater had the doses been higher and durations of treatment longer.
Symptoms such as poor emotional regulation, irritability, anxiety and general mood, showed the greatest improvement. Greater effects were noted in those with more severe symptoms and in those with conditions of neurodiversity such as ADHD and ASD, but again showing greater improvement in emotional regulation, mood and anxiety, rather than the core diagnostic criteria.
Using a ‘targeted’ approach with single vitamins or minerals does not show the same level of response in mental health conditions as a broad spectrum approach, which makes logical sense given the fact that so many vitamins and minerals are crucial for the metabolic pathways involved in brain function.
So what supplements should I give my child? Or take myself?
If your child is suffering from a mental health condition, your first step is contacting your GP.
If you would like advice on supplementation whilst awaiting treatment or alongside treatment, or if you have any questions, then please do get in touch. I can advise on dietary changes and the best supplements (usually those used in the actual trials) and regimens for individual symptoms and circumstances.
If you found this article interesting, subscribe below for more in the series – next will be a review on gut health and the ever-emerging evidence of its relationship to mental health.
References
These are the main references used, but a full list is available on request:
Expert reaction to a review paper on the ‘serotonin theory of depression’. Science Media Centre. 2022.https://www.sciencemediacentre.org/expert-reaction-to-a-review-paper-on-the-serotonin-theory-of-depression/ (accessed 13/9/ 2022).
Sarris J, Ravindran A, Yatham LN, Marx W, Rucklidge JJ, McIntyre RS, Akhondzadeh S, Benedetti F, Caneo C, Cramer H, Cribb L, de Manincor M, Dean O, Deslandes AC, Freeman MP, Gangadhar B, Harvey BH, Kasper S, Lake J, Lopresti A, Lu L, Metri NJ, Mischoulon D, Ng CH, Nishi D, Rahimi R, Seedat S, Sinclair J, Su KP, Zhang ZJ, Berk M. Clinician guidelines for the treatment of psychiatric disorders with nutraceuticals and phytoceuticals: The World Federation of Societies of Biological Psychiatry (WFSBP) and Canadian Network for Mood and Anxiety Treatments (CANMAT) Taskforce. World J Biol Psychiatry. 2022 Mar 21:1-32. doi: 10.1080/15622975.2021.2013041. Epub ahead of print. PMID: 35311615.
Johnstone JM, Hughes A, Goldenberg JZ, Romijn AR, Rucklidge JJ. Multinutrients for the Treatment of Psychiatric Symptoms in Clinical Samples: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2020 Nov 4;12(11):3394. doi: 10.3390/nu12113394. PMID: 33158241; PMCID: PMC7694278.
Jacques Duff, Chapter Fourteen – Nutrition for ADHD and Autism, Editor(s): David S. Cantor, James R. Evans,
Clinical Neurotherapy, Academic Press, 2014, Pages 357-381, ISBN 9780123969880, https://doi.org/10.1016/B978-0-12-396988-0.00014-3.
Kennedy DO. B Vitamins and the Brain: Mechanisms, Dose and Efficacy–A Review. Nutrients. 2016 Jan 27;8(2):68. doi: 10.3390/nu8020068. PMID: 26828517; PMCID: PMC4772032.
Giménez-Palomo A, Dodd S, Anmella G, Carvalho AF, Scaini G, Quevedo J, Pacchiarotti I, Vieta E, Berk M. The Role of Mitochondria in Mood Disorders: From Physiology to Pathophysiology and to Treatment. Front Psychiatry. 2021 Jul 6;12:546801. doi: 10.3389/fpsyt.2021.546801. PMID: 34295268; PMCID: PMC8291901.
Johnstone JM, Hughes A, Goldenberg JZ, Romijn AR, Rucklidge JJ. Multinutrients for the Treatment of Psychiatric Symptoms in Clinical Samples: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2020 Nov 4;12(11):3394. doi: 10.3390/nu12113394. PMID: 33158241; PMCID: PMC7694278.
Derbyshire E. Brain Health across the Lifespan: A Systematic Review on the Role of Omega-3 Fatty Acid Supplements. Nutrients. 2018 Aug 15;10(8):1094. doi: 10.3390/nu10081094. PMID: 30111738; PMCID: PMC6116096.
Appleton KM, Voyias PD, Sallis HM, Dawson S, Ness AR, Churchill R, Perry R. Omega-3 fatty acids for depression in adults. Cochrane Database Syst Rev. 2021 Nov 24;11(11):CD004692. doi: 10.1002/14651858.CD004692.pub5. PMID: 34817851; PMCID: PMC8612309.
Veselinović A, Petrović S, Žikić V, Subotić M, Jakovljević V, Jeremić N, Vučić V. Neuroinflammation in Autism and Supplementation Based on Omega-3 Polyunsaturated Fatty Acids: A Narrative Review. Medicina (Kaunas). 2021 Aug 28;57(9):893. doi: 10.3390/medicina57090893. PMID: 34577816; PMCID: PMC8464922.
Noro, F., Marotta, A., Bonaccio, M. et al. Fine-grained investigation of the relationship between human nutrition and global DNA methylation patterns. Eur J Nutr 61, 1231–1243 (2022). https://doi.org/10.1007/s00394-021-02716-8
Taylor, M.R., Chuang, C., Carrasco, K.D., Rucklidge, J. J. (2018). Dietary and
Micronutrient Treatments for Children with Neurodevelopment Disorders. Current Developmental Disorders Reports, 5, 243-252.
Stevens, A., Rucklidge, J. J., & Kennedy, M. A. (2017). Epigenetics, nutrition and mental health. Is there a relationship? Nutritional Neuroscience, 21, 602-613.
Rucklidge, J. J., Harris, A., & Shaw, I. (2014). Are the amounts of vitamins in commercially available dietary supplement formulations relevant for the management of psychiatric disorders in children? New Zealand Journal of Medicine, 127, 73-85
Popper, C. W. (2014). Single-Micronutrient and Broad-Spectrum Micronutrient Approaches for Treating Mood Disorders in Youth and Adults. Child and Adolescent Psychiatric Clinics of North America, 23(3), 591-672. doi:10.1016/j.chc.2014.04.001
Rucklidge, J. J., Johnstone, J., & Kaplan, B. J. (2009). Nutrient supplementation approaches in the treatment of ADHD. Expert Review of Neurotherapeutics, 9(4), 461-476.
Popper, C., Kaplan, B. J., & Rucklidge, J. J. (2017). Single and Broad-Spectrum Micronutrient Treatment in Psychiatric Practice. In Complementary and Integrative Treatments in Psychiatric Practice. Edited by Patricia L. Gerbarg, M.D., Philip R. Muskin, M.D., Richard P. Brown, M.D. American Psychiatric Press, Washington, D.C
(pp 75-101)
Rucklidge, J. J., Johnstone, J. J., & Kaplan, B. J. (2021). Nutrition is an essential foundation for optimizing mental health. Evidence Based Practice in Child and Adolescent Mental Health, 6(1), 131-154. http://dx.doi.org/10.1080/23794925.2021.1875342
Blampied, M., Bell, C., Gilbert, C., & Rucklidge, J. J. (2020). Broad spectrum micronutrient formulas for the treatment of symptoms of depression, stress and/or anxiety: a systematic review. Expert Review of Neurotherapeutics, 20 (4), 351–371. https://www.tandfonline.com/doi/full/10.1080/14737175.2020.1740595
